
Blog
What is Tibial Interlocking Nail and How Does It Work?
The Tibial Interlocking Nail is a crucial medical device used in orthopedic surgeries. It provides strong internal support for fractured tibia bones. This method ensures proper alignment and stability during the healing process.
Many surgeons favor the Tibial Interlocking Nail for its effectiveness. It allows for earlier mobility, which may improve recovery times. Patients often experience less pain, as this system minimizes the need for external casts. However, challenges exist. Not all fractures are ideal for this technique.
Complications can arise. These may include infection or improper alignment of the nail. Surgeons must carefully evaluate each case. Understanding the unique anatomy of the patient is vital. The Tibial Interlocking Nail is not a one-size-fits-all solution; each situation requires thoughtful consideration.
What is a Tibial Interlocking Nail?
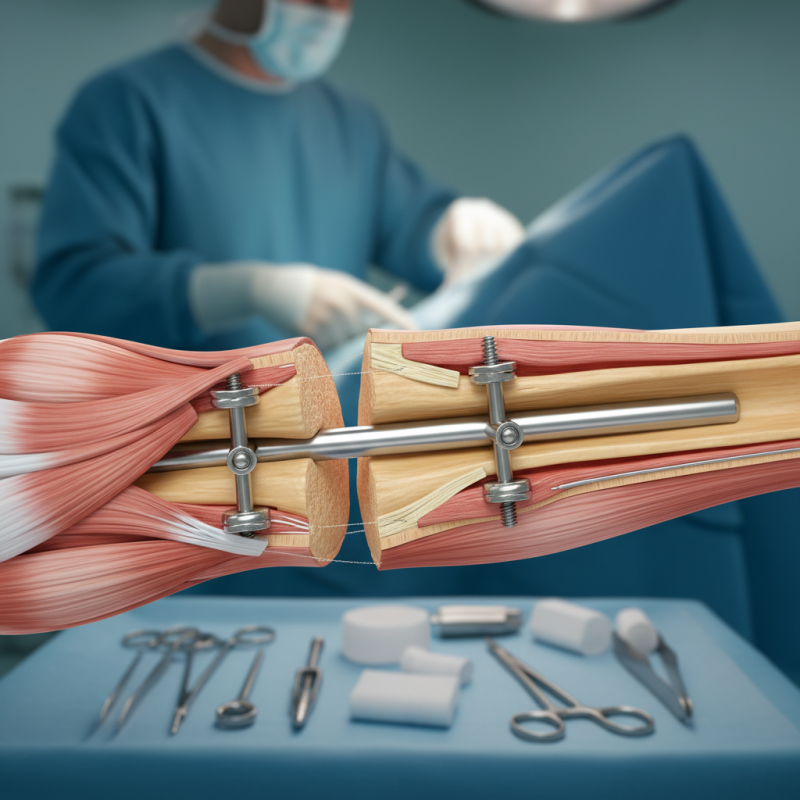
A tibial interlocking nail is a medical device used in orthopedic surgery. It stabilizes a broken tibia, which is the larger bone in the lower leg. The nail is inserted into the center of the tibia through small incisions. This helps guide the healing process by keeping the bone fragments aligned.
The design of the tibial interlocking nail allows for flexible placement. Surgeons can use different entry points based on each patient's needs. The device is locked in place using screws that secure it within the bone. This enhances stability during recovery. However, the procedure requires precision. Incorrect placement can lead to complications, like improper alignment.
Recovery after using a tibial interlocking nail varies. Some patients heal quickly, while others face challenges. Factors like age, overall health, and adherence to rehabilitation play significant roles. Patients must engage in physical therapy to regain strength. While this device is effective, it is not foolproof. There can be infections or hardware failure. Constant monitoring is necessary to ensure a successful outcome.
Tibial Interlocking Nail Usage in Orthopedic Surgery
This chart illustrates the distribution of tibial interlocking nail procedures performed across different age groups. The data indicates that procedures are most common among individuals aged 36-45, with a notable decrease in older age groups.
The Surgical Indication for Tibial Interlocking Nails
Tibial interlocking nails are used for treating complex tibial fractures. These nails are commonly indicated when there is instability in fractures. Fractures caused by high-energy trauma often require this method. It provides strong internal fixation, ensuring proper alignment during healing.
Surgeons consider several factors before using tibial interlocking nails. Age, bone quality, and the type of fracture are crucial. Open fractures with skin loss pose a challenge. Infections can complicate the situation. The decision to use these nails should involve careful assessment.
Patients often express concerns about the recovery process. Pain management and physical therapy are vital components. Overcoming fear of movement is important. Improved healing can be slow but steady. Awareness of potential issues can help in planning effective treatment. Understanding each step fosters teamwork between the patient and surgical team.
Mechanism of Action in Fracture Stabilization
The tibial interlocking nail is a specialized device used in orthopedic surgery. It stabilizes fractures in the tibia, the larger bone in the lower leg. This nail is inserted into the medullary canal of the bone. Then, it locks into place with screws. This mechanism provides strong support and helps maintain proper alignment during healing.
The stabilization process involves both compression and interlocking action. When the screws are tightened, they pull the fracture ends together. This reduces movement and promotes healing. Bone cells can rebuild around the nail, providing a solid framework. However, achieving the ideal alignment can be challenging. Surgeons must carefully assess each case.
Tips: Always follow your surgeon's advice after the procedure. Rehabilitation plays a crucial role in recovery. Gradual weight-bearing is often recommended to avoid stress on the nail and bone. Regular follow-ups are essential to monitor progress and make necessary adjustments.
Clinical Outcomes and Success Rates in Tibial Nail Procedures
Tibial interlocking nailing is a popular procedure for treating tibial fractures. Its success largely depends on various clinical outcomes. Surgeons assess factors like alignment and stabilization of the bone during the healing process. Generally, studies show that this procedure has a favorable success rate, particularly in non-complex fractures.
Patients often report improved mobility and reduced pain after the surgery. However, not every case results in complete recovery. Some report complications such as infection or delayed healing. These issues might stem from the initial injury or the surgical technique applied. Understanding these potential pitfalls helps refine future procedures.
Inherent challenges exist within tibial nail procedures. Patients’ healing abilities vary; some may face obstacles that hinder recovery. Surgeons must continuously adapt and modify techniques based on individual cases. Striking a balance between innovation and safety is crucial in improving outcomes. Each case provides opportunities for learning and adjustments in practice.
Complications and Considerations in Tibial Nail Surgery
Tibial nail surgery can come with various complications. Infection is one of the primary concerns. It may occur at the incision site or deeper within the bone. Preventive measures are essential. Patients must monitor their surgical site for signs of swelling or redness. Regular follow-ups with the surgeon can help catch issues early.
Fractures might not heal correctly. Malalignment or nonunion could happen if the nail is not positioned perfectly. Patients should adhere to post-operative care closely. Engagement in physical therapy can promote healing. Keep weight off the leg as directed. This helps avoid unnecessary strain on the healing process.
Tips: Always communicate openly with your doctor about pain. It’s crucial to manage discomfort efficiently. Keeping a pain diary can aid in understanding your recovery. Consider mental wellness too. Surgery can be mentally challenging. Finding support can make a difference. Reflection on your journey can lead to better coping strategies.